During a typical cath lab procedure, x-ray scanning is performed to guide the physician and technologists. For the patient, this may amount to insignificant radiation exposure. However, the physicians and their staff do not leave the lab after one patient. For them, the process just repeats itself—often, for many years.
“I'm sure at one point we're going to find out that this x-rays fluoro that we are using is going to have bad side effects on us.”
– Samer Abbas, Interventional Cardiologist
Interventional physicians experience some of the highest rates of radiation exposure within the medical profession,1 due in large part to fluoroscopy – a gold standard for visualization in endovascular procedures.
The cumulative effects of fluoroscopy exposure are only now becoming evident, with recent data correlating increased radiation exposure with linear increases in the risk of cancer.2 Interventional healthcare providers and their staff don’t always realize these effects. Mostly because the cumulative effects have a biological latency of more than 10 years.3
Interventional Physicians Have the Highest Radiation Exposure of all Professions 4,5

With an interest in reducing the risks that interventionists face, new technologies have demonstrated the ability for physicians to improve both patient and operator safety.
“The fact that we're able to image without using any photons or without using any dangerous photons, is a significant advantage.”
– Scott Brannan, Interventional Radiologist
Reducing Radiation Exposure: Risks Associated with Cath Lab Radiation
LE Revascularization X-Ray Exposure 6,7,8,9,10
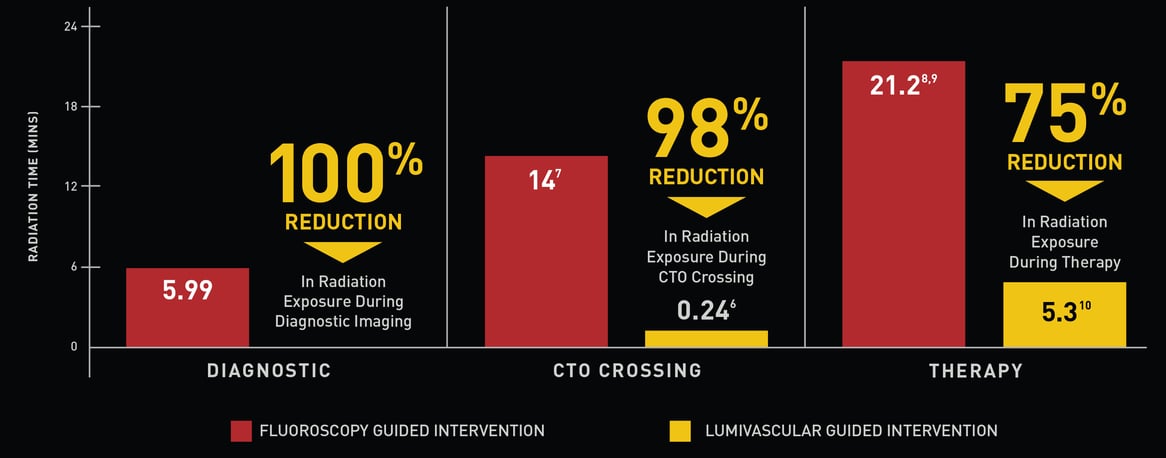
Additional peer reviewed evidence presented at LINC 2016 retrospectively measured fluoroscopic times of patients undergoing OCT-guided CTO crossing.10 In this presentation, Dr. Marianne Brodmann demonstrated a quick learning curve with dramatic reduction in total fluoroscopy and contrast loads administered, when compared with published data (Figure 2). 10,11,12,13,14,15
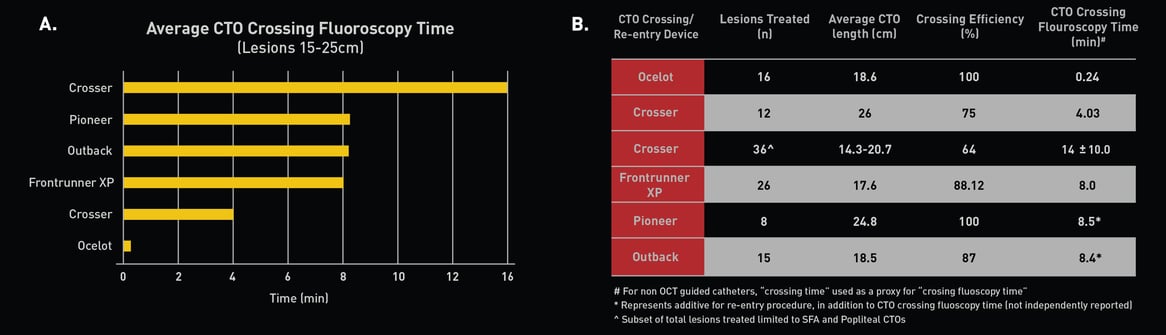 Figure 2. (A) Fluoroscopy time measurements comparing various atherectomy/crossing devices during Revascularization; 12,13,14 (B) Total number of lesions treated per crossing device, including CTO length, crossing efficiency, and total fluoroscopy time.10,11,12,13,14,15,16
Figure 2. (A) Fluoroscopy time measurements comparing various atherectomy/crossing devices during Revascularization; 12,13,14 (B) Total number of lesions treated per crossing device, including CTO length, crossing efficiency, and total fluoroscopy time.10,11,12,13,14,15,16
OBESITY & RADITATION: WHAT IS KNOWN
- Obesity has become more prevalent among patients with PAD, practically CLI and patients undergoing undergoing catheterization.17,18
- Increasing patient body mass index results in higher patient radiation doses during procedures.18
- The greatest source of physician and staff radiation exposure during catheterization comes from scatter radiation emitted from the patient, which itself is proportional to patient radiation dose
Operator exposure during atherectomy – A device comparison
Total case radiation dosages were analyzed retrospectively in procedures performed using OCT-guided atherectomy versus cases completed using fluoroscopy guided atherectomy. Results demonstrated a significant 63% reduction in median fluoroscopic exposure across all procedures completed using OCT guidance (p<0.05) (Figure 3).15,16 The clinical implications of sustained reduction in exposure to radiation is significant for operators and clinical staff with long-term endovascular career exposure.
Conclusion
To date, the lack of advanced imaging on endovascular catheters has perpetuated the reliance on angiography.
These results suggest that OCT-guided CTO crossing and OCT-guided atherectomy enable physicians to significantly reduce both patient and operator radiation exposure. Importantly, these critical reductions are appreciated in both new and old users to the technology, highlighting a fast learning curve.19
“Information attained from within the vessel, can produce safer and more effective results than if we rely solely on traditional X-ray fluoroscopic imaging.”
– Edward Pavillard, Vascular Surgeon
Learn more about OCT-Guided Atherectomy & CTO Crossing
To find a representative in your area, please click here.
References
-
- Venneri, et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council's Biological Effects of Ionizing Radiation VII Report. Am Heart J. 2009;157(1):118-124.
- The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37(2-4):1-332.
- Gerber, et al. Radiation dose and safety in cardiac computed tomography. Cardiol Clin. 2009;27(4):665-677.
- International Atomic Energy Agency (IAEA)
- Zakeri, et al. Biological effects of low-dose ionizing radiation exposure in interventional cardiologist. Occup Med (Lond). 2010 Sep;60(6):464-9
- Davis T. No-Fluoroscopy Crossing of Chronic Total Occlusions Using Ocelot Optical Coherence Tomography Guided Catheter. Vascular Disease Management. 2015.
- Staniloae, Cezar S., et al. "Endoluminal treatment of peripheral chronic total occlusions using the Crosser® recanalization catheter." Journal of Invasive Cardiology 23.9 (2011): 359.
- Laird, John R., et al. "Excimer laser with adjunctive balloon angioplasty and heparin‐coated self‐expanding stent grafts for the treatment of femoropopliteal artery in‐stent restenosis." Catheterization and Cardiovascular Interventions 80.5 (2012): 852-859.
- Roberts, David, et al. "Effective endovascular treatment of calcified femoropopliteal disease with directional atherectomy and distal embolic protection: final results of the DEFINITIVE Ca++ trial." Catheterization and Cardiovascular Interventions 84.2 (2014): 236-244.
- Brodmann, M. Lumivascular Case Series, LINC 2016
- Loomis, et al. Mortality from brain cancer and leukaemia among electrical workers. Br J Ind Med. 1990;47(9):633-638.
- Grayson JK. Radiation exposure, socioeconomic status, and brain tumor risk in the US Air Force: a nested case-control study. Am J Epidemiol. 1996;143(5):480-486.
- Blettner, et al. Medical exposure to ionising radiation and the risk of brain tumours: Interphone study group, Germany. Eur J Cancer. 2007;43(13):1990-1998.
- Davis TP. Lumivascular Approach to Crossing Chronic Total Occlusions Without Fluoroscopy. Paper presented at: Transcatheter Cardiovascular Therapeutics (TCT)2014; Washington, DC.
- Bannazadeh, et al. Patterns of procedure-specific radiation exposure in the endovascular era: impetus for further innovation. J Vasc Surg. 2009;49(6):1520-1524.
- Davis TP. Optical Coherence Tomography (OCT) Enables the Reduction in Fluoroscopic Exposure During Endovascular Atherectomy. Paper presented at: Transcatheter Cardiovascular Therapeutics (TCT)2016; Washington, DC.
- Hicks, et al. Associations of Obesity With Incident Hospitalization Related to Peripheral Artery Disease and Critical Limb Ischemia in the ARIC Study. J Am Heart Assoc. 2018 Aug 21;7(16)
- Madder, et al. Patient Body Mass Index and Physician Radiation Dose During Coronary Angiography. Circ Cardiovasc Interv. 2019;12
- Schwindt A. Lower extremity revascularization using optical coherence tomography guided directional atherectomy. Final results of the EValuatIon of the PantheriS OptIcal COherence Tomography ImagiNg Atherectomy System for use in the Peripheral Vasculature (VISION) Study. 2016.