OCT Guided Atherectomy Following Antegrade and Retrograde Posterior Tibial CTO Crossing Via Bridging Collateral for CLI Limb Salvage
Sean Janzer MD
Einstein Medical Center, Philadelphia, PA
CASE DETAILS
A 73-year-old female with past medical history was referred with diabetes mellitus type 2, hypertension, and CAD. The patient has Category 5 Rutherford critical limb ischemia with ulceration of the left foot. Diagnostic angiography revealed a denovo ostial 70mm posterior tibial (PT) artery chronic total occlusion (CTO). The anterior tibial (AT) artery had significant proximal disease with a mid-vessel CTO. The peroneal artery had significant proximal disease, however, was patent distant to the ankle.
PLANNED INTERVENTION
1. Ipsilateral antegrade access using a 7Fr sheath.
2. A CTO crossing wire was advanced antegrade into the peroneal and translated across a bridging collateral artery distal to the PT reconstitution, tracked retrograde back up the PT, through the CTO via the true lumen to establish in-line flow. The wire was externalized back through ipsilateral sheath.
3. Recanalization was achieved using OCT-guided directional atherectomy with Pantheris catheter
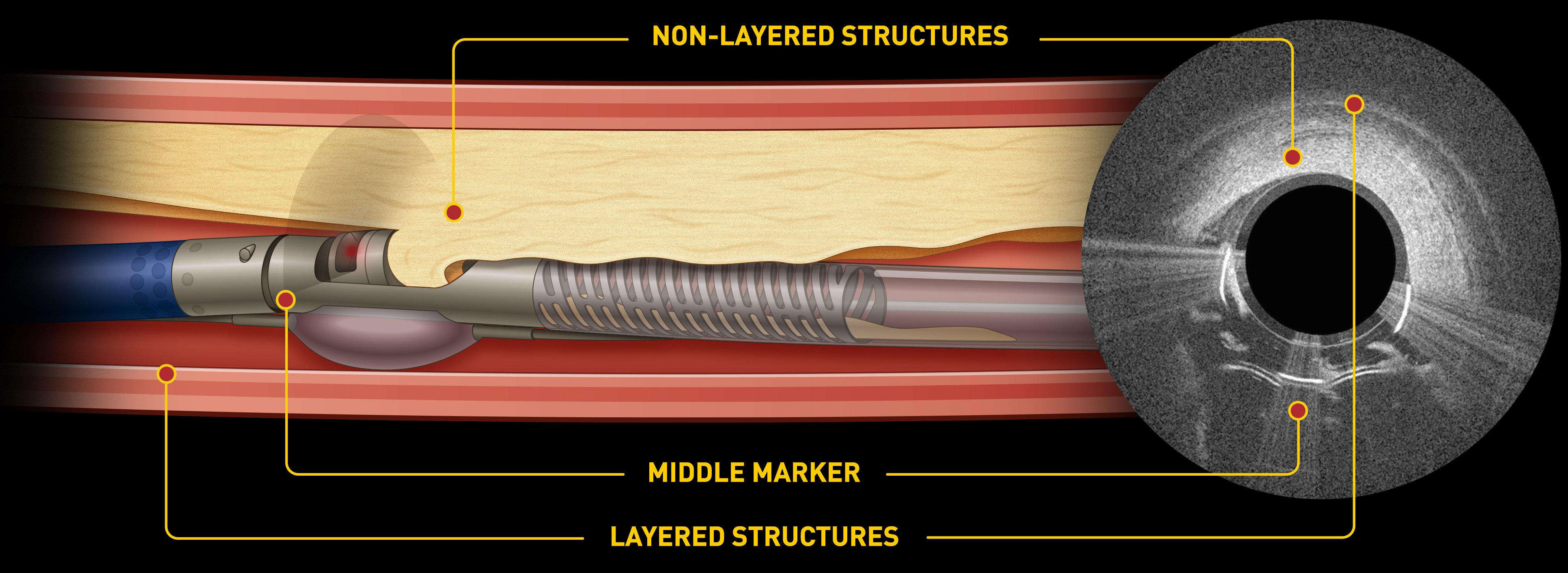
PANTHERIS - OCT GUIDED ATHERECTOMY
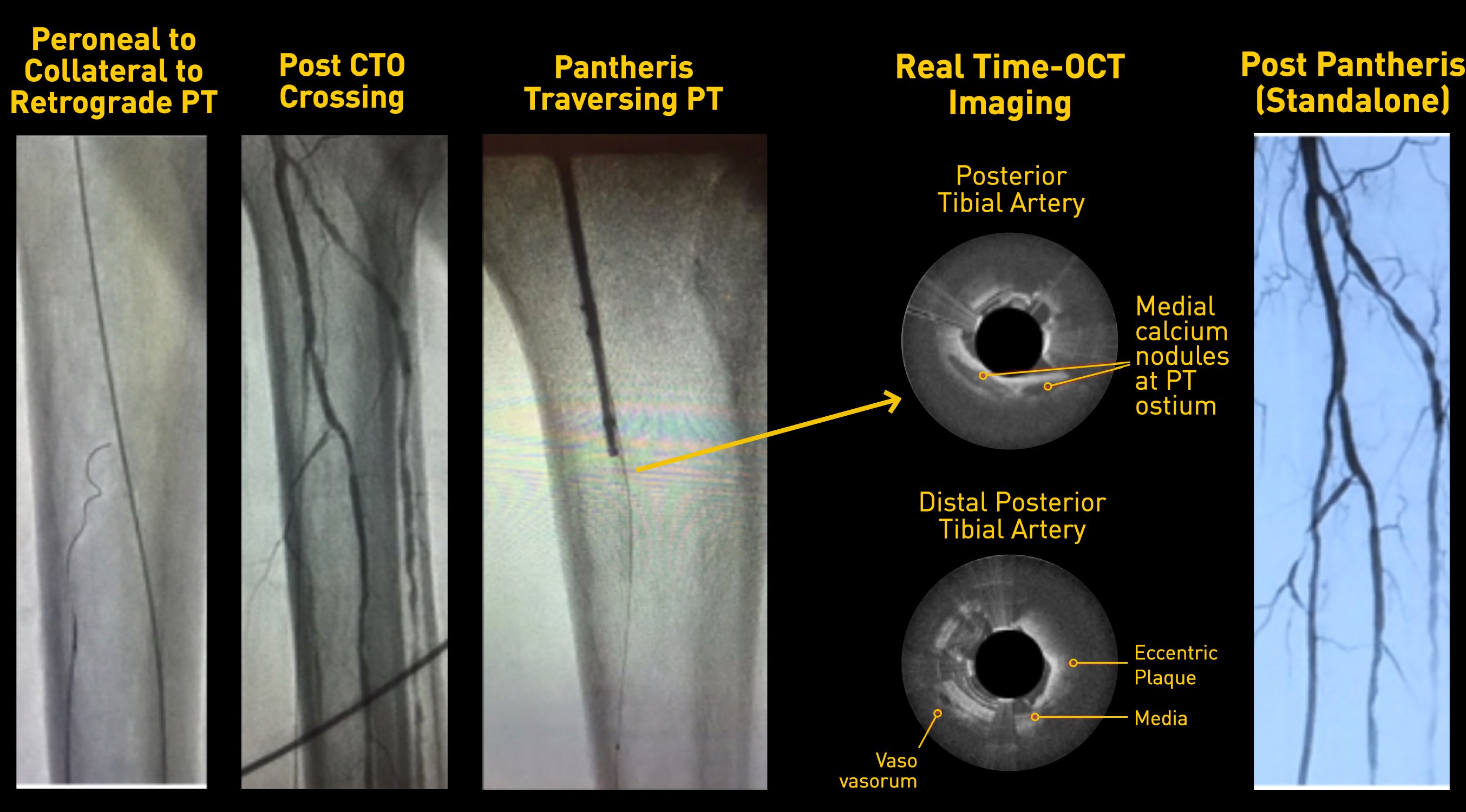
CTO CROSSING & OCT-GUIDED REVASCULARIZATION
POST ATHERECTOMY
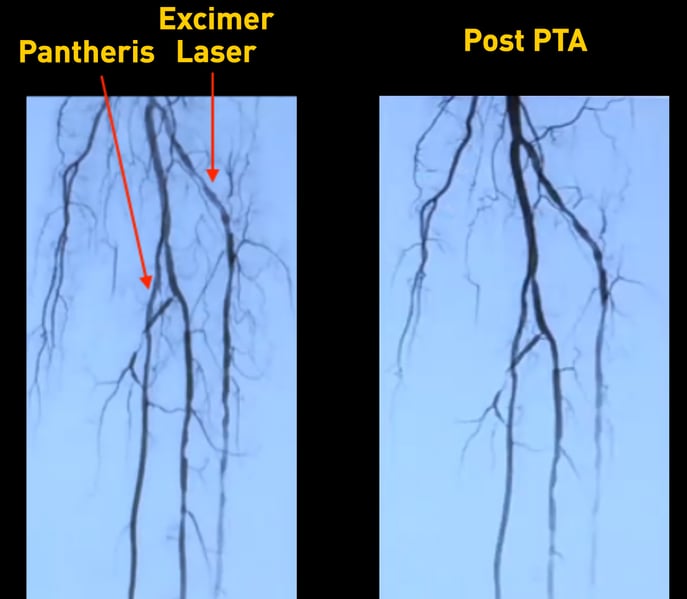
Laser was used to treat AT as the stenosis extended to ankle. Pantheris was used to treat PT because of occlusion with significant disease burden. The middle image compares standalone laser versus standalone Pantheris.
TAKE HOME MESSAGE
1. Using OCT, semi-lunar medial calcification was noted at the PT CTO proximal cap; focal lateral fibrinous disease at the mid-CTO section with larger amounts of preserved media and inferior focal luminal calcification at the distal reconstitution site.
2. OCT guided directional atherectomy resulted in dissection free flow with <10% residual stenosis. No adjunctive therapy was required.
3. OCT guided atherectomy proves to be a beneficial choice when recanalizing severe lesion type, due to its ability to discern the nature of the eccentric occlusive disease.
LINC2017
